Tracheoesophageal fistula & esophageal atresia treatment
Find a GI specialistWhat is tracheoesophageal fistula (TEF)?
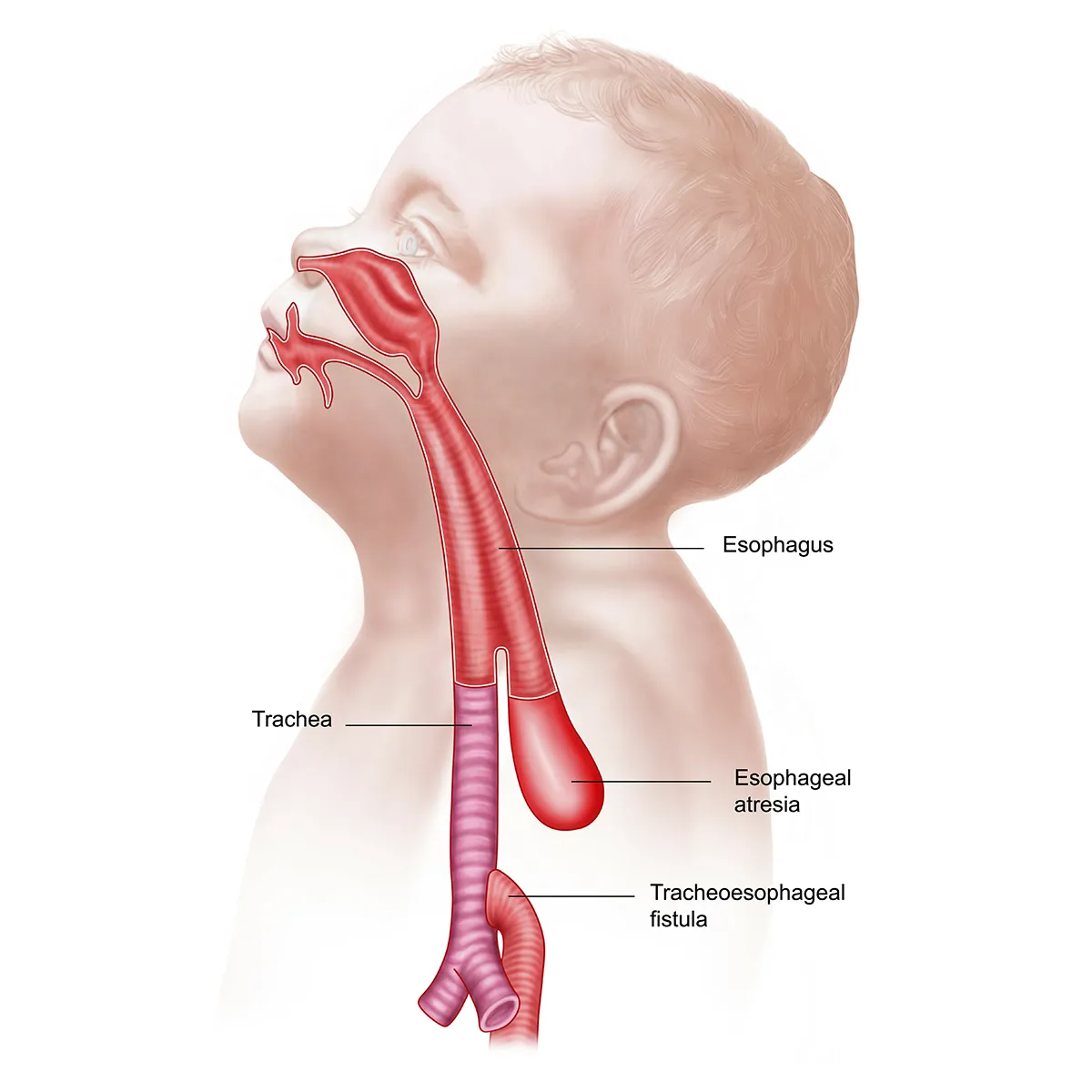
As your baby develops, the esophagus and trachea begin as one tube and separate before birth. In rare cases, they don’t separate correctly, and the trachea stays attached to the esophagus. This is known as tracheoesophageal fistula, and it’s usually not diagnosed until after birth.
With tracheoesophageal fistula, air may enter the stomach and cause it to be distended. Or contents of the esophagus (milk and secretions) may be inhaled. This can cause choking, pneumonia and even death in serious cases.
Older children or adults with cancer could develop tracheoesophageal fistula when a tumor invades both the trachea and esophagus, but this is rare.
What is esophageal atresia (EA)?
Atresia occurs when a body part fails to develop normally and closes off or narrows when it shouldn’t.
When your baby is born with esophageal atresia, it means their esophagus doesn’t reach the stomach correctly.
The most common way this happens is when the top part of the esophagus has a closed end and the bottom part of the esophagus connects to the trachea. This is a combination of an atresia and a tracheoesophageal fistula. However, esophageal atresia can also occur without a fistula. In most types of EA, your baby won’t be able to swallow food into their stomach. They may also have trouble breathing.
Unlike tracheoesophageal fistula, esophageal atresia can sometimes be detected during pregnancy. If your baby does have this condition, our doctors will work quickly to begin treatment as soon as your baby is born. If it’s not diagnosed before birth, esophageal atresia symptoms are usually obvious as soon as your baby tries to feed.
Tracheoesophageal fistula and esophageal atresia causes
Causes of either of these conditions are unknown, and they don’t appear to be inherited. Researchers believe that many factors may be involved.
Conditions related to esophageal atresia
Esophageal atresia has been associated with several genes and genetic disorders, including trisomy 13 (Patau syndrome), trisomy 18 (Edwards syndrome) and trisomy 21 (Down syndrome).
About half of all babies born with tracheoesophageal fistula and esophageal atresia will have related anomalies known as VACTERL association, also referred to as VATER syndrome. In other rare cases, a genetic condition known as CHARGE syndrome may be present. These are groups of birth defects that are often found together. Birth defects of the eyes, ears, kidneys, intestines, heart, stomach, muscles or bones may be involved in these syndromes.
In rare instances, some infants with tracheoesophageal fistula and esophageal atresia may also be born with a hole in their diaphragm, known as congenital diaphragmatic hernia.
Your care team screens for these conditions and will coordinate the safest order of treatments. Treatment for tracheoesophageal fistula and esophageal atresia may be delayed if a more serious condition is present.
Your doctors will explain your baby’s individual condition completely and keep you informed at every stage of their treatment.
What are the symptoms of tracheoesophageal fistula and esophageal atresia?
While these conditions usually occur together, tracheoesophageal fistulas and esophageal atresia each have their own symptoms.
Identifying these symptoms early is crucial to ensure your child has a full recovery.
Symptoms of tracheoesophageal fistula
Symptoms of tracheoesophageal fistula may not appear right away, so a diagnosis may not come until the early weeks of your baby’s life. Coughing while feeding and lung infections are the most common symptoms.
Esophageal atresia symptoms
Symptoms of esophageal atresia will vary depending on how much of the esophagus is missing and whether they also have tracheoesophageal fistula.
Symptoms may include:
- Bluish skin color
- Coughing or choking during feeding
- Difficulty breathing
- Frothy white bubbles in your baby’s mouth
Because this condition involves how your baby swallows food and breastmilk, symptoms typically appear soon after birth.
Risks associated with tracheoesophageal fistula and esophageal atresia
These birth defects require immediate treatment, and your baby may face long-term or short-term risks even after surgery.
Potential risks include:
- Breathing problems
- Swallowing and feeding difficulties
- Gastroesophageal reflux (GERD) and esophagitis
- Esophageal strictures or leaks after surgery
- Recurrent fistulas (TEF‑specific)
- Airway weakness or collapse
- Long‑term gastrointestinal and respiratory challenges
Diagnosis of tracheoesophageal fistula and esophageal atresia
To diagnose tracheoesophageal fistula and esophageal atresia, your baby’s doctor will observe their symptoms and perform tests that show the location of the defects. Some of the tests they may use are:
- X-rays of the chest and abdomen
- Endoscopy of esophagus: Inserting a scope (a clear, thin tube with a camera at the end) into the esophagus to see how far it goes and whether there’s a connection to the trachea
- Bronchoscopy of trachea and lungs: Inserting a scope into the trachea to see if there are connections to the esophagus
Esophageal atresia and tracheoesophageal fistula types
Your child’s doctor will determine the severity of these birth defects by identifying the type of esophageal atresia and tracheoesophageal fistula. Because tracheoesophageal fistula and esophageal atresia occur together, they are classified using a combined system.
These types include:
- Type A: Esophageal atresia without tracheoesophageal fistula. The esophagus ends in two separate blind pouches with no connection to the trachea.
- Type B: The upper esophageal pouch connects to the trachea, but the lower esophagus does not. It is extremely rare.
- Type C: This is the most common type, accounting for 85% of all cases. The lower esophagus connects to the trachea, while the upper esophagus ends in a blind pouch.
- Type D: An extremely rare type where both the upper and lower esophagus connect to the trachea at different points.
- Type E (H type): Tracheoesophageal fistula without atresia. The esophagus is intact, but an H-shaped fistula connects to the trachea. Because babies can still swallow, this type is harder to diagnose.
Tracheoesophageal fistula and esophageal atresia treatment
Once your child’s tracheoesophageal fistula and esophageal atresia type has been identified, our team will begin a treatment plan focused on supporting your baby’s recovery and long-term health.
Your baby will need to be admitted into the neonatal intensive care unit (NICU) at an Aurora facility. Given this condition affects how your baby eats and breathes, this is important. An outpatient treatment plan is not possible.
Until your baby’s defects can be corrected, they’ll need to be fed artificially through an IV with total parenteral nutrition or through a feeding tube inserted directly into the stomach. Once surgery is complete and your baby has recovered, you can begin breastfeeding again if you have chosen to do so.
Esophageal atresia surgery
Your baby will need surgery to separate the trachea and esophagus or to repair any holes. Depending on your baby’s condition, several surgeries may be needed over a period of weeks.
Esophageal atresia treatment focuses on creating an esophagus long enough to reach the stomach.
If the gap between the upper and lower esophagus is small enough, they’ll be stitched together using primary anastomosis, a surgical technique where two ends are sewn back together.
If the esophagus is too short or if a segment is missing, surgeons will use a more complex procedure known as a jejunal interposition. This is when a piece of the small intestine (the jejunum) is used to bridge the gap between the esophagus and the stomach. Part of your baby’s intestines will be safely removed without impacting their long-term digestion. It’s often an effective alternative when the esophagus is missing.
Advanced esophageal atresia treatment
When the gap between the upper and lower esophagus is too large for these surgeries, an internal traction procedure is used to lengthen the esophagus segments. Sutures are placed inside the chest to encourage gradual stretching over several days. Once they are closer, the esophagus is stitched together.
This procedure is often used for esophageal atresia types A and B when the gap between the esophagus is too large for other treatment options.
Navigating this process and watching your child go through this can be scary, but our team is committed to supporting your child’s recovery. The esophageal atresia surgery success rate is very high, with most babies making a full recovery.
Tracheoesophageal fistula treatment
Tracheoesophageal fistula is repaired at the same time as an esophageal atresia. During surgery, the doctor will close the abnormal connections between the airway and esophagus to allow for normal breathing and feeding.
The exact surgery chosen depends on the tracheoesophageal fistula type. If a fistula has occurred on its own without esophageal atresia, surgical repair is performed to divide the fistula and close the esophageal sides.
Treatment may include staged repairs, minimally invasive techniques and additional procedures to support feeding or breathing as your child recovers.
Is TEF a surgical emergency?
Yes. Both tracheoesophageal fistula and esophageal atresia are considered emergencies and require urgent treatment. Surgical repair of the trachea and esophagus takes place within hours after giving birth. This is especially important since this condition affects your baby’s ability to feed and breathe.
Post-op care after surgery
Before you restart feeding, your baby may have an esophagram. This is a contrast X‑ray that shows whether the surgical connection has healed without a leak and if the esophagus is open or narrowed. This is typically done about five to 10 days after surgery and helps the team safely advance feeding.
Taking your baby home after surgery
Your baby will remain in the NICU after surgery for several weeks. Most babies will be discharged once they can do the following:
- Eat by mouth or feed safely without a gastrostomy tube (feeding tube)
- Gain weight
- Breathe on their own
- Recover from anesthesia and surgical repair
- No longer need intensive monitoring
Our team at Aurora Health Care works hard to support your child’s recovery, and they may need to see a specialist for follow-up care. These visits will focus on monitoring breathing, feeding and esophageal function.
Get care
We help you live well. And we’re here for you in person and online.