Esophageal varices
Find a GI specialistEsophageal varices can be a serious, sometimes life-threatening, result of advanced liver disease. At Aurora Health Care, our expert esophageal varices specialists tap into the latest diagnostic tools and treatments to provide the best possible care.
What are esophageal varices?
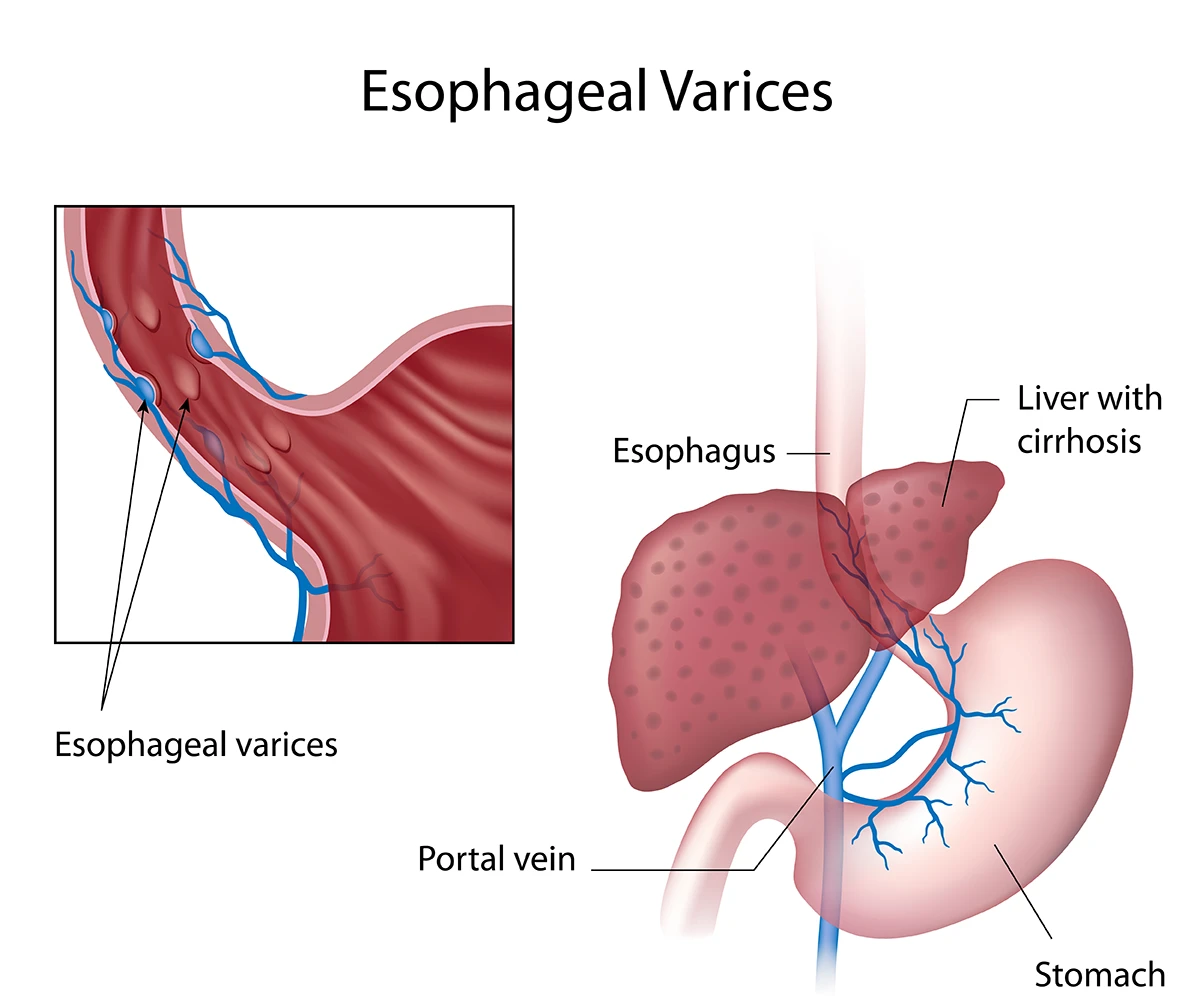
Esophageal varices are enlarged veins in the esophagus. When these veins become blocked, they restrict blood flow to the liver.
Esophageal varices are swollen veins in the lower part of your esophagus. They usually occur when severe liver disease like cirrhosis slows blood flow through your liver. This causes pressure to increase in your esophageal veins.
Your liver plays a vital role in filtering your blood before it goes to your heart and other organs. When you have liver disease, blood can’t flow through your liver as easily as it should. This puts pressure in your portal vein – a main blood vessel that gets blood from your esophagus and digestive organs to your liver. This increased pressure has a ripple effect on the veins in your esophagus, which begin swelling.
When these veins become too swollen, they bleed and even rupture. This poses significantly greater risks to your body and is what your doctors will work to prevent when treating esophageal varices.
Esophageal varices causes
Most esophageal varices are caused by cirrhosis of the liver. Cirrhosis causes a condition known as portal hypertension, which then causes esophageal varices.
Other less common causes include:
- Blood clots in the portal vein
- Certain infections that affect blood flow to the liver
- Birth defects
Risks for developing esophageal varices
Protecting your liver is the best way to lower your risk of developing esophageal varices. The more damaged and scarred your liver becomes, the greater your risk.
Certain activities and conditions increase your risk of liver disease, including:
- Excessive alcohol intake
- Obesity
- Diabetes
- High triglycerides
- Chronic hepatitis B or hepatitis C infections
- Nonalcoholic fatty liver disease
- Genetic predispositions
- Contributing conditions, such as schistosomiasis or Budd-Chiari syndrome, which can increase the risk of bleeding
Esophageal varices symptoms
Esophageal varices symptoms are usually unnoticeable until the esophageal varices rupture. Signs you may have ruptured varices include:
- Throwing up blood
- Black, tar-like or bloody stool
- Feeling light-headed or dizzy
Signs of advanced liver disease may also be common. These symptoms include yellow skin (jaundice), abdominal pain or dark urine.
If you experience any of these symptoms, schedule an appointment with an Aurora specialist. If you see blood in your vomit or stool, call 911 and seek emergency care immediately.
Diagnosing esophageal varices
If you have liver disease, your doctor will likely recommend an upper endoscopy to check for bleeding or swollen veins. Since esophageal varices don’t cause symptoms until they bleed, these routine checks are especially important to prevent internal bleeding or ruptured veins.
During the endoscopy, a flexible tube with a light and camera will be inserted through your mouth. You’ll be sedated, so you will be sleepy and won’t feel anything. The doctor will guide the endoscope down your throat to look for swollen veins.
Occasionally a capsule endoscopy, CT scan or ultrasound may be used, but these are not usually preferred because they don't show varices as clearly.
Esophageal varices grading system
When diagnosing varices, the team at Aurora Health Care will classify them as either small or large. While more complex grading systems can also be used, this simple, two-grade system follows the guidelines from the American Association for the Study of Liver Diseases (AASLD).
Since large varices are more likely to bleed, the treatment is much more aggressive than small ones.
Esophageal varices treatment
An esophageal varices rupture will cause severe gastrointestinal bleeding if it isn’t treated quickly. For that reason, treatment focuses on stopping or preventing the veins from bleeding and rupturing.
The type of treatment depends on the size and severity of your veins. Our team at Aurora Health Care may take one or more of the following steps:
Esophageal varices medication
Beta blockers, a type of blood pressure medication, are often the first line of defense to prevent bleeding. They are ideal because they reduce pressure in your portal vein, which is usually the main cause of esophageal varices. By alleviating pressure in this vein, you reduce the swelling in your esophageal veins.
Banding esophageal varices
If your veins are bleeding or at high risk for bleeding, your doctor might recommend esophageal varices banding. This is a very common outpatient procedure done during an upper endoscopy.
You will be sedated for the procedure, so you won’t feel anything or experience any pain. The doctor will insert the endoscope into your mouth and will gently push the tube into your esophagus.
The doctor then places an elastic band around the swollen part of your vein. This blocks blood flow to that section of the vein, causing it to lose its blood supply and shrink. After about a week, the tied-up tissue naturally detaches, and both it and the rubber band pass through your digestive tract. This is a normal and safe process with minimal risk.
Endoscopic treatment is sometimes repeated over several weeks until all the varices disappear. Recurrence is possible if pressure in the portal vein remains high.
Shunts for high-risk bleeding
If more advanced treatment is needed for severe cases, it usually focuses on treating portal hypertension, as that’s frequently the underlying cause of the bleeding esophageal varices.
Transjugular intrahepatic portosystemic shunt (TIPS) is the most common procedure. A shunt is placed in the liver to create a new pathway for blood to flow through your liver. This stops pressure from building in both the portal vein and in your esophagus.
While often a last resort, this procedure is highly effective. Most patients find it a successful option with minimal risks when paired with medication and lifestyle changes.
Life expectancy for esophageal varices
Esophageal varices are a sign of an underlying liver condition like cirrhosis or portal hypertension. Your outlook depends largely on how healthy your liver is and whether the varices have bled.
When the condition is monitored regularly and managed with preventive measures, such as avoiding alcohol and taking beta-blockers, many people significantly reduce their risk of bleeding.
Large varices carry a much higher risk, and bleeding esophageal varices is a medical emergency. Our team at Aurora Health Care will work quickly to stabilize bleeding and prevent complications. If you think your varices have ruptured, call 911 immediately.
Are esophageal varices curable?
Esophageal varices can be treated, but they can’t be permanently cured. Because they form as a result of high pressure in the veins around your liver, varices can return as long as that pressure remains.
In some early liver conditions, treating liver disease may help the varices shrink. In more advanced stages of liver disease, the varices often come back and only go away permanently after a liver transplant.
Esophageal varices prevention
The best way to prevent esophageal varices from developing or rupturing is to keep your liver healthy. Lifestyle changes and healthy daily habits can help, including:
- Avoid alcohol: Limit how much alcohol you drink, as it’s a major cause of liver damage.
- Follow a healthy diet: Choose lean meats, whole grains, fruits and vegetables. Limit foods high in saturated fat, which contribute to liver strain.
- Reduce exposure to chemicals: Wear gloves and protective equipment when using cleaning products, solvents or paints.
- Maintain a healthy weight: Carrying excess weight can strain your liver.
- Protect yourself from viral hepatitis: Get vaccinated for hepatitis A and hepatitis B, practice safe sex and see a doctor if you have hepatitis C.
Get care
We help you live well. And we’re here for you in person and online.