Hemorrhoid treatment
Find a GI specialistHemorrhoids and your colorectal health are no cause for embarrassment or discomfort. At Aurora Health Care, your doctor and care team will give you clear, accurate information about what to do and how to get rid of them.
What are hemorrhoids?
A hemorrhoid is simply an inflamed or swollen vein around the anus (the opening that lets feces exit the body) or inside the rectum. Hemorrhoids around the anus are called external hemorrhoids. Those that form inside the rectum are called internal hemorrhoids.
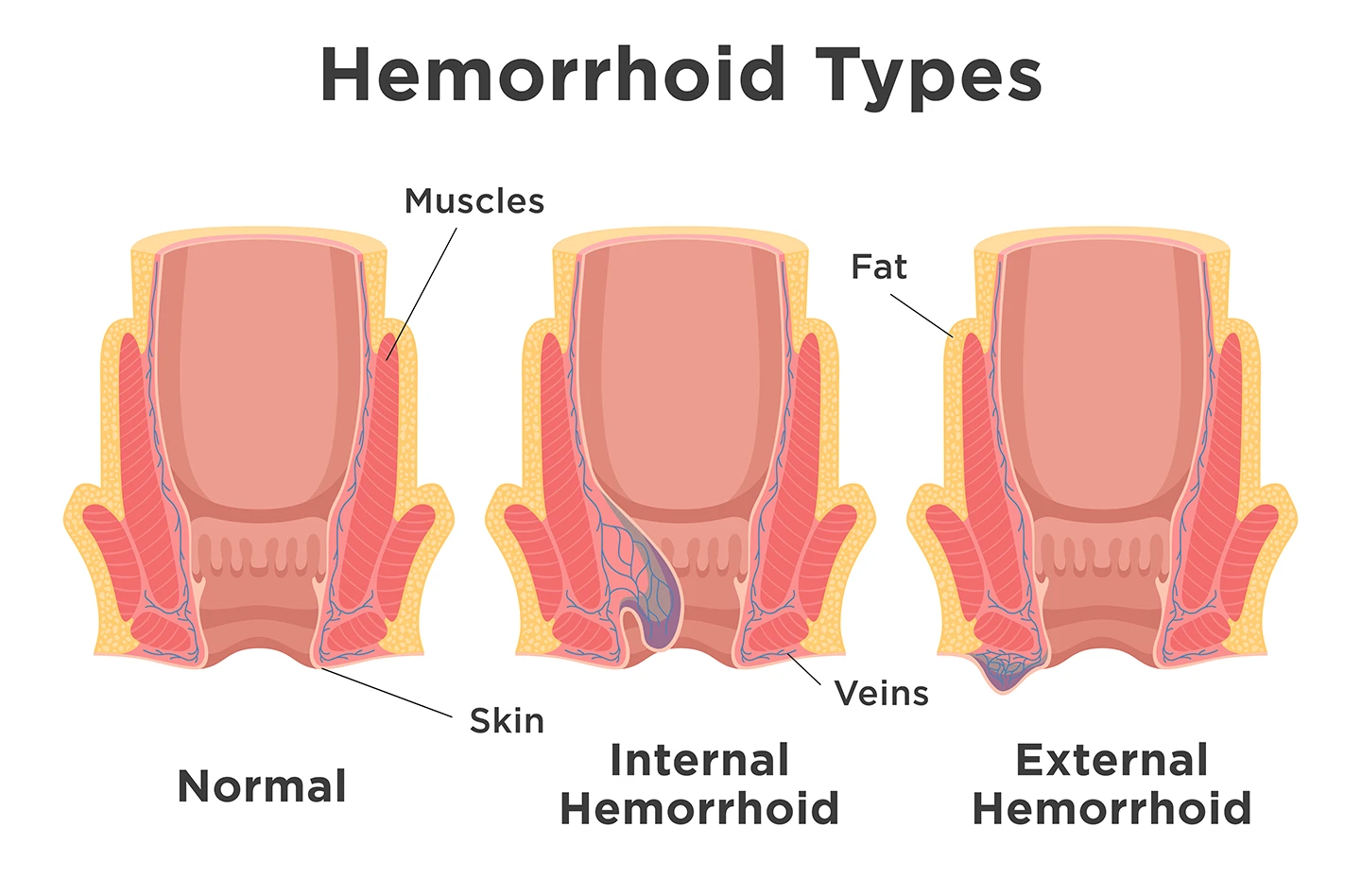
Hemorrhoids can be internal or external, depending on where they form.
What are the different types of hemorrhoids and what do they look like?
Hemorrhoids fall under four different types. No matter what kind of hemorrhoid you have, they’re often annoying and uncomfortable, and sometimes extremely painful.
Internal hemorrhoids
An internal hemorrhoid is mostly colored red because it forms on the mucous membrane that lines the inside of the anus. They are often not serious and tend to go away on their own. If left unchecked, they can swell, leading to discomfort, itching, burning or rectal bleeding. You usually won’t see an internal hemorrhoid and you may not even know you have it unless a doctor tells you about it after an exam or a procedure like a colonoscopy.
Prolapsed hemorrhoids
A prolapsed hemorrhoid occurs when an internal hemorrhoid of the mucosal lining swells enough to stick out of the anus. They appear as soft, red lumps. Prolapsed hemorrhoids are categorized into four grades.
- Grade 1: Not prolapsed at all
- Grade 2: Bulge outside the anus during a bowel movement or straining, but will retract (return inside the anus) by itself
- Grade 3: Prolapsed and bulging outside the anus even when not straining, and do not retract on their own. You may be able to carefully push them back inside, or they may require treatment.
- Grade 4: Prolapsed and bulging outside of the anus at all times. These are likely painful and cannot easily be pushed back in. They usually require treatment.
External hemorrhoids
An external hemorrhoid looks skin-colored or reddish. It makes a hard, tender bump, and it may itch or be covered in mucus. As opposed to prolapsed hemorrhoids, which begin inside the body and may swell outside of it, external hemorrhoids form on the outside of your anus and do not change their position.
Thrombosed hemorrhoid
If either an internal or external hemorrhoid develops a blood clot inside it, it may take on a blue, purple, grey, black or dark brown color (depending on your skin color). A hemorrhoid with a blood clot inside it is called a thrombosed hemorrhoid and can cause severe pain when walking or standing.
What are common hemorrhoid symptoms?
Symptoms of hemorrhoids may include:
- Soreness or burning pain
- Itchiness or irritation
- Bulging of a vein
- One or more hard, tender lumps near the anus
- Bleeding
If you notice blood in your stool, on your toilet paper or in the toilet, contact your doctor. While hemorrhoids are one of the most common causes of rectal bleeding, it can also be a sign of other conditions. Your doctor will want to check for anal fissures, ulcerative colitis, Crohn’s disease or some types of cancer. Treatments for these conditions are different from each other, so your doctor will want to rule out other explanations before moving forward.
What are potential hemorrhoid complications?
Complications from hemorrhoids are rare, but can include:
- Anemia: A drop in healthy blood cells due to chronic blood loss.
- Infection: A condition caused by harmful microorganisms, including bacteria, viruses, fungi or parasites.
- Skin tags: Skin that remains after a blood clot inside a hemorrhoid is reabsorbed.
- Strangulated hemorrhoid: When part of an internal hemorrhoid prolapses and its blood supply is cut off by the muscles of the anus. This can be very painful.
What are potential hemorrhoid causes and risk factors?
We don’t know exactly why hemorrhoids form. But we do know some things that make you more likely to develop them:
- A diet low in fiber
- Aging
- Anal sex
- Chronic constipation or diarrhea
- Genetics (some people inherit a tendency to develop hemorrhoids)
- Lifting heavy things (particularly when it’s frequent)
- Obesity
- Pregnancy
- Smoking
- Straining during bowel movements
- Standing or sitting for long periods of time
How can you prevent hemorrhoids?
You can prevent hemorrhoids and their complications with a few lifestyle changes. Don’t strain or hold your breath while pooping, which puts pressure on rectal veins. Properly clean your anus after going to the bathroom using soft, unscented toilet paper or wipes.
Other ways to prevent hemorrhoids include:
- Add more fiber to your diet like whole grains, fruits, vegetables and legumes
- Drink lots of fluids; water is best
- Avoid sitting on the toilet for more than five minutes
- If you have to poop, don’t delay or stool may become harder to pass
- Exercise regularly
- Maintain a healthy weight to reduce rectal pressure
- Try fiber supplements like psyllium or methylcellulose
- During pregnancy, Kegel exercises can help strengthen pelvic muscles
What are some of the best hemorrhoid treatments at home?
At-home remedies for hemorrhoids include:
- Pain relievers like aspirin, ibuprofen or acetaminophen
- Sitz baths: sitting in warm water for 15 minutes two to three times a day
- Topical creams such as hydrocortisone
- Applying an ice pack or cold compress
If any of these hemorrhoid treatments don’t improve your symptoms within a week or if you have severe pain or bleeding, you should contact your doctor. They’ll be able to verify whether you have hemorrhoids or another condition that has similar symptoms. Aurora providers can confirm a diagnosis and offer a variety of treatments depending on the severity of your case.
How are hemorrhoids diagnoised?
Your doctor will start with a thorough physical, including asking about your general health history and your symptoms. They’ll ask if you’ve been doing anything to treat the pain and whether or not those things have helped.
They’ll do a physical exam and check the appearance of any external hemorrhoids. They may do a digital rectal exam by putting on gloves, applying lubrication and inserting a finger into your rectum to feel for tenderness or lumps and check muscle tone.
Depending on what they find, they may also use an anoscope (short plastic tube) or a sigmoidoscope (flexible lighted tube) to look at the colon.
How will my provider treat hemorrhoids?
If your provider diagnoses you with hemorrhoids, they may recommend that you try some at-home treatments first. If those don’t offer relief, or if your case is more severe, they may recommend one of the following treatments.
Nonsurgical hemorrhoid treatments
Bleeding and persistent hemorrhoids can be treated with minimally invasive procedures such as:
- Rubber band ligation: Your doctor puts one or two small medical-grade rubber bands around the base of a hemorrhoid to cut off its blood flow. You may need more than one banding hemorrhoid treatment to get the hemorrhoid to shrink and fall off.
- Sclerotherapy: Your doctor injects a chemical solution into the hemorrhoid that cuts off its blood supply, causing the hemorrhoid to shrink. Any pain is minimal.
- Cryotherapy: Your doctor applies a cooled gas or liquid to freeze the external hemorrhoid, which then shrinks and falls off.
Hemorrhoid surgery
Surgery is usually recommended for large hemorrhoids, bleeding or prolapsed internal hemorrhoids, or those that haven’t responded to other hemorrhoid treatments. These hemorrhoid treatments are usually outpatient procedures but sometimes require an overnight hospital stay. Procedures include:
- Excisional hemorrhoidectomy: This hemorrhoid treatment includes surgical removal, where your doctor makes incisions around the hemorrhoid and removes it while you’re under general anesthesia. You may have pain after the procedure and may need to take it easy for as long as two weeks, but the surgery has a high rate of lasting success.
- Stapled hemorrhoidopexy: This method of hemorrhoid treatment doesn’t require an incision. Instead, using a device inserted through a tube into your anus, your doctor removes tissue around the hemorrhoid. The hemorrhoid is lifted and the tissue is stapled back into place. Blood flow to the hemorrhoid is cut off, and it shrinks within four to six weeks. Stapled hemorrhoidopexy takes about 30 minutes under general anesthesia. This hemorrhoid treatment is usually less painful than hemorrhoidectomy and lets you get back to your regular activities faster.
- Thrombectomy: A thrombectomy is a tiny incision your doctor makes to drain a clot and relieve the pressure on your skin.
Get care
We help you live well. And we’re here for you in person and online.