Vericoceles
Find a urologistMale reproductive health can be an uncomfortable topic to discuss with your doctor. At Aurora Health Care, our team of compassionate urologists are here to help and understand your reproductive issues and get you the proper care when you need it.
We treat a variety of male reproductive issues with empathy, including erectile dysfunction, infertility and varicoceles.
What is a varicocele?
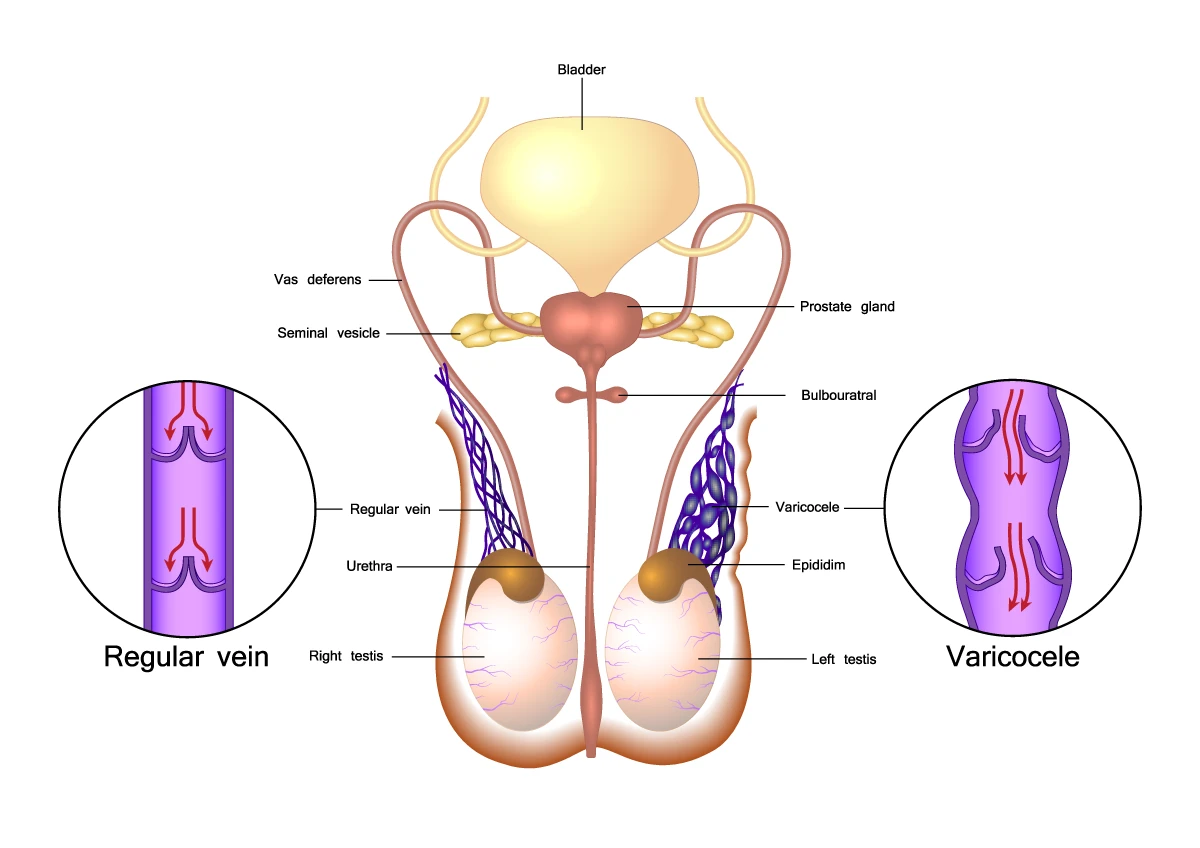
A varicocele is a condition where veins within the pouch of skin that holds the testicles (the scrotum) become swollen. It occurs when the valves within the veins that regulate blood flow in the spermatic cord don't function correctly, causing blood to pool and the veins to swell.
This leads to the formation of a varicose vein, similar to varicose veins that can occur in the legs.
Typically, varicoceles cause mild symptoms, including swelling of the scrotum and pain in the testicles.
You may not notice any symptoms. If a varicocele causes significant discomfort or affects fertility, medical treatment may be considered.
Varicocele risk factors
Varicoceles are common in males and people assigned male at birth. About one in five men are affected by varicoceles. You are more likely to be affected by varicoceles in the left side of your scrotum than the right or both sides.
While the exact cause of varicoceles is unknown, several factors are believed to contribute to varicocele development, including:
- Defective valves: The valves within the testicles are responsible for sending blood toward the heart. When they become weak or malfunction, blood accumulates in the veins, causing swelling and forming a varicocele.
- Genetics: Varicoceles tend to run in families, suggesting a genetic predisposition.
- Hormonal changes: Hormonal fluctuations, particularly during puberty, are believed to play a role. Increased hormone activity may lead to dilation of the testicular veins, contributing to varicocele formation.
- Physical activity: Prolonged standing or sitting can put pressure on the veins in the scrotum, causing them to dilate and potentially contributing to varicocele development.
Although less common, varicoceles can also be caused by external factors like tumors, kidney disease or injuries that disrupt blood flow in the scrotal region.
Complications of varicoceles
Most varicoceles go away with proper treatment. However, larger varicoceles may cause complications such as low testosterone and infertility.
Low testosterone may shrink the size of the testicles, reduce sex drive, cause depression and decrease muscle mass.
Varicocele symptoms
Varicoceles often do not cause any symptoms, especially in mild cases. However, when symptoms do occur, they might include:
- Dull pain or discomfort
- A visible swelling or lump in the scrotum
- Aching or throbbing in the scrotum
- Infertility
It's important to note that many varicoceles are asymptomatic and might be discovered incidentally during a physical exam. If you suspect you have a varicocele or are experiencing any symptoms in the scrotum, contact your provider to schedule an appointment.
Diagnosing varicoceles
The varicocele diagnosis process involves a combination of a physical exam, medical history review and a review of your symptoms. During the physical exam, your doctor may perform an exam of your scrotum.
Your provider may also order other tests to accurately diagnose varicoceles, including:
- Digital imaging: An ultrasound provides a visual of the veins in the testicles and is the most common test used to diagnose varicoceles.
- Blood tests: A blood test is used to check hormone levels, including testosterone and follicle-stimulating hormones (FSH), which affects sexual development in children.
- Semen analysis: A semen analysis is often ordered to check the health of the sperm and to see if a varicocele is affecting fertility.
Grades of a varicocele
Your doctor will use a grading system to describe the severity and size of varicoceles.
- Grade 0: A varicocele is visible on an ultrasound, but not physically detectable.
- Grade I: A varicocele can be felt on the scrotum when performing a Valsalva maneuver, which is where you stand up, take a deep breath, hold your nose and mouth closed and strain to push air out.
- Grade II: A varicocele can be felt without using a Valsalva maneuver.
- Grade III: The varicocele is clearly visible and can be felt.
Varicocele treatment options
Varicocele treatment is recommended based on the severity (grade) of your varicocele. For less severe varicoceles, your provider may recommend at-home treatment that includes the use of ice packs, making lifestyle changes or taking over-the-counter medications such as naproxen and ibuprofen for pain relief from varicoceles.
If your varicoceles are severe, your doctor may recommend a varicocelectomy, a surgical procedure to redirect blood flow to healthy veins in the scrotum.
Get care
We help you live well. And we’re here for you in person and online.